
Estrogen and Progesterone
Multiple studies have highlighted the impact of estrogen and progesterone on melasma:
-
Pregnancy and Oral Contraceptives: The condition is notably prevalent among pregnant women and those using oral contraceptives, suggesting a hormonal trigger.
-
Estrogen Receptors on Melanocytes: Estrogen is believed to stimulate melanogenesis through its receptors on melanocytes, leading to increased pigmentation.
-
Clinical Observations: A study involving 66 female melasma patients found that 72.7% had elevated estrogen levels, underscoring its potential role in the condition’s pathogenesis.
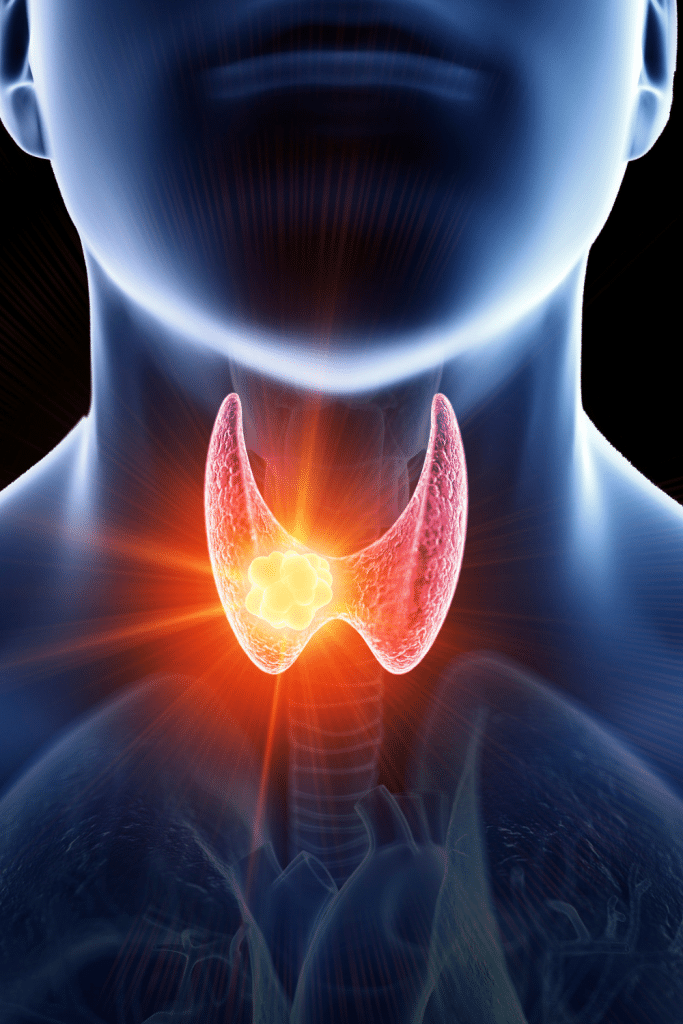
Thyroid Hormones
Thyroid dysfunction has also been associated with melasma:
-
Increased Incidence: Patients with thyroid disease exhibit a higher prevalence of melasma, indicating a possible link between thyroid hormones and skin pigmentation.
-
Autoimmunity Factors: Autoimmune thyroid disorders may influence melanocyte activity, contributing to hyperpigmentation.
Cortisol and Stress
Chronic stress, leading to elevated cortisol levels, may exacerbate melasma:
-
Oxidative Stress: Increased cortisol can induce oxidative stress, affecting melanocyte function and promoting pigmentation.
-
Inflammatory Response: Stress-related inflammation may alter skin homeostasis, facilitating melasma development.
Genetic Predisposition
Genetics also play a crucial role in melasma susceptibility:
-
Family History: Approximately 30% of patients report a familial occurrence of melasma, suggesting hereditary factors.
-
Ethnic Predilection: Individuals with Fitzpatrick skin types III to V, particularly those of African, Asian, or Hispanic descent, are more prone to developing melasma.
Pathogenesis: Beyond Hormones
While hormones are pivotal, other factors contribute to melasma’s pathogenesis:
-
UV Radiation: Sun exposure remains a primary trigger, as ultraviolet light stimulates melanocyte activity, leading to increased melanin production.
-
Skin Inflammation: Procedures causing skin irritation or inflammation can precipitate melasma in predisposed individuals.

Management Strategies
Addressing hormonal influences is vital in melasma management:
-
Hormonal Evaluation: Assessing and managing hormonal imbalances, such as thyroid dysfunction, can be beneficial.
-
Sun Protection: Regular use of broad-spectrum sunscreen is essential to prevent UV-induced melanogenesis.
-
Topical Agents: Agents like hydroquinone, retinoids, and azelaic acid can help reduce pigmentation.
-
Advanced Therapies: Procedures such as chemical peels, laser therapy, and microneedling have shown efficacy in treating melasma.
Conclusion
Melasma’s multifactorial etiology encompasses hormonal, genetic, and environmental components. Understanding the hormonal underpinnings, particularly the roles of estrogen, progesterone, and thyroid hormones, is crucial for effective management. Further research is warranted to elucidate these complex interactions and develop targeted therapies.

